Cover Story
Vol 10, Issue 1
Lipedema: Understanding a Complex Condition
By Jennifer Boggs | Feature Story
Letter from the Editor
Empowering patients through education
Medicine is based on science, but there’s an art to it too. When diagnosing patients at the Vein Healthcare Center, we use tools like duplex ultrasound and venous reflux tests to determine whether vein disease is present and to what degree. We also talk with each patient about how changes in their legs feel, their family history, and other health factors. The art is looking at a patient and their experience holistically.
In this issue of Vein Health News, we explore a condition called lipedema. Though it’s not venous in nature, there is often a co-occurrence with venous issues and lymphedema.
Lipedema is estimated to affect 10 to 17 million people in the United States, primarily women. The true prevalence is likely higher due to widespread underdiagnosis. The good news is that in 2021, a group of experts in the U.S. released a “consensus guideline” to standardize care for this diagnosis. Evolving scientific research is helping to increase knowledge of and about the condition.
At our practice we see a number of patients who have lipedema, and we do everything we can to provide knowledge to understand the condition. Education and resources are essential for managing lipedema — including the difficult emotions that can arise after diagnosis.
There is no cure for lipedema, but there have been advancements in management, including graduated compression, Manual Lymphatic Drainage (MLD), medications like GLP-1 and GIP agonists, and surgical intervention. There are ways for people with lipedema to feel better and improve their quality of life. You can read about one woman’s experience in our regular column, “One Patient’s Perspective.”
The art of medicine also involves conveying complex information to patients so that they can become their own advocates. We hope that the information in this issue can be a way for both patients and providers to better understand a complicated condition.
- Dr. Cindy Asbjornsen, D.O., FAVLS, RPhS, ABVLM, FACPh
Lipedema is NOT obesity. It is an increase of fat tissue that is hard to lose, despite diet, exercise, or bariatric surgery.
Medical diagnoses are not always obvious, especially when symptoms are complex, varied, and can easily be mistaken for other conditions. Lipedema (pronounced lai-puh-dee-muh or lip-puh-dee-muh) is one such condition. It is often confused with lymphedema, obesity, or cellulite. Adding to the complexity, lipedema can co-occur with other conditions, such as venous disease.
Although often misdiagnosed or underdiagnosed, lipedema is quite common. Lipedema is a clinical diagnosis, and there are currently no blood tests or imaging studies that can confirm it. Research into the diagnosis and management of lipedema continues. In 2021, a group of experts released a "consensus guideline" creating a standard of care for lipedema in the U.S. This and other research are helping to advance understanding towards early diagnosis, treatment, and hopefully one day, a cure.
What is lipedema?
Lipedema is a loose connective tissue disorder that results in an abnormal buildup of adipose (fat) cells in the limbs. These cells settle into certain areas of the body, most often in the hips and legs—disproportionately more significantly than in the upper body (although lipedema sometimes affects the arms and lower trunk). Areas affected by lipedema tend to be symmetrical, while the hands and feet are typically spared.
Someone with lipedema may experience pain, tenderness, swelling, or easy bruising of the affected areas. The intensity and frequency of pain can vary. The condition may be accompanied by an unusual lumpy or fibrous texture within the fat tissue that can feel like peas or walnuts beneath the surface of the skin.
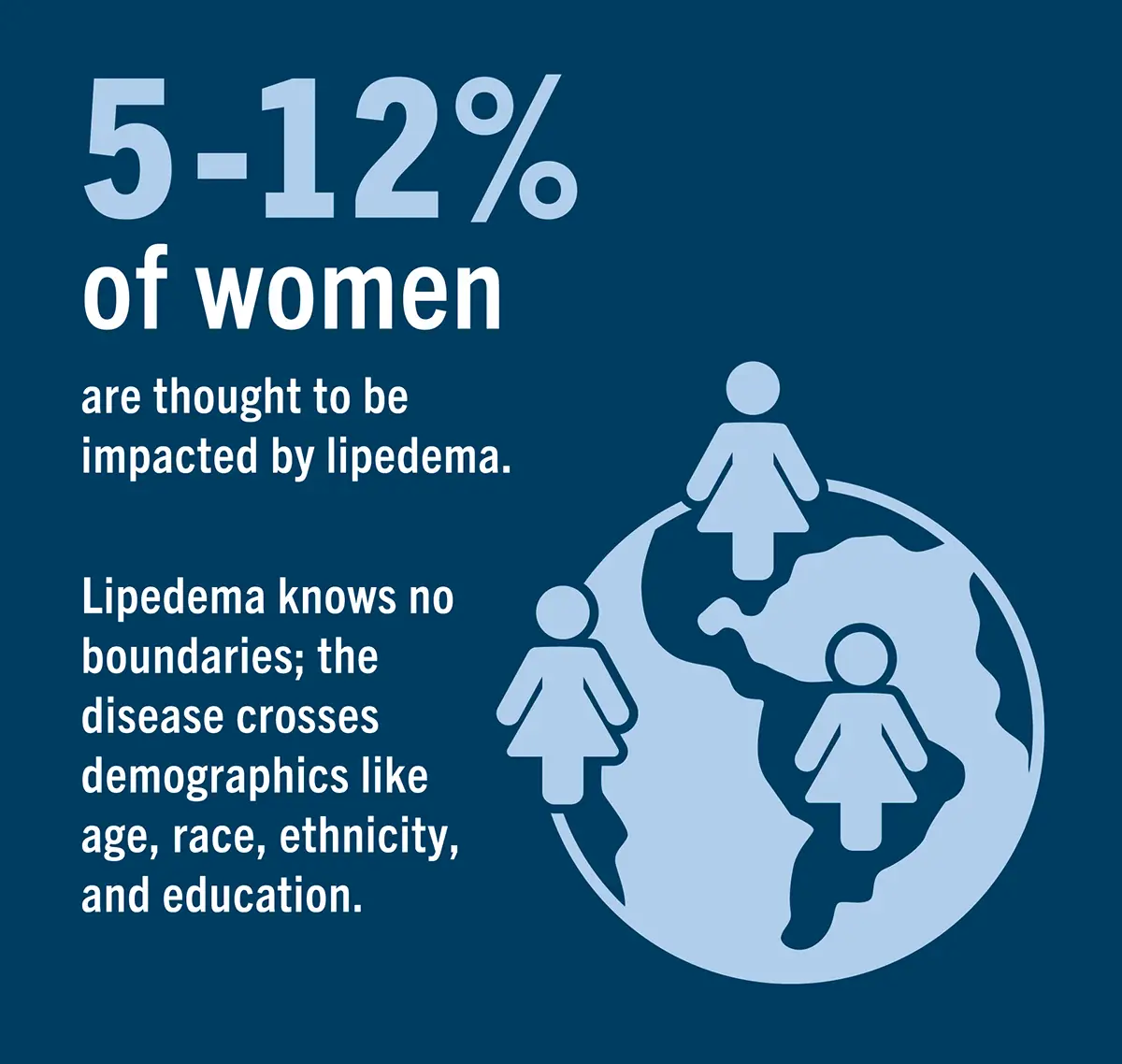
The cause of lipedema is unknown, though it is believed to be hereditary. Research is underway to determine the biological role of genetics, hormones, inflammation, and metabolism in the condition’s development. Several genes have been implicated, most notably the mutated gene AKR1C1. Lipedema occurs almost exclusively in women, and about 5-12 percent of women in the U.S. are affected. Studies have shown that it often runs in families on the mother’s side.
Signs and symptoms
Symptoms of lipedema vary from person to person and may worsen over time. Lipedema can develop at any age, but most symptoms seem to develop (or worsen) during periods of hormonal change such as puberty, pregnancy, or perimenopause, or sometimes when a person takes hormonal birth control. Major trauma, gynecological surgery, and significant periods of stress can also trigger lipedema.
Common symptoms include:
- Excess fat that builds up in the lower extremities, causing buttocks, hips, thighs, and calves to become significantly larger than the upper body
- Fibrous tissue within the fat that may feel like lumps beneath the skin
- Pain, ranging from mild to severe, that is constant or occurs only with pressure
- Swelling or dimpling around the affected areas
- A sensation of heaviness or fatigue in the legs
- Skin that bruises easily (ecchymosis)
- Feet/hands are typically spared, sometimes appearing like an ankle or wrist “cuff”
What lipedema is not
For many people, lipedema is not the first diagnosis offered for their array of symptoms. They may think that their weight gain or shape of their bodies is due to obesity or something else. To that end, let’s first discuss the conditions that lipedema is not.
Lipedema is often confused with obesity, but is quite different. Obesity-related fat occurs throughout the body, while in lipedema, the fat occurs in the limbs (and sometimes lower trunk), typically sparing the hands and feet. People with early-stage Lipedema typically do not have conditions that are more commonly associated with obesity such as diabetes, high cholesterol, or high blood pressure.
Another distinction is that lipedema is resistant to diet, exercise, and bariatric surgery. While the disease can be exacerbated by obesity, there are many women who have lipedema and are not obese.
Lipedema is often mistaken for lymphedema, a chronic condition that causes swelling in body tissues due to a buildup of lymph fluid. The swelling in lymphedema often affects only one side of the body and includes the hands and feet. Lymphedema can be diagnosed with the help of imaging or genetic tests. There are no definitive tests for lipedema, so diagnosis is based on patient history, physical examination, and ruling out other disorders. Lymphedema can occur secondary to lipedema, as the accumulation of fat cells in the tissues can lead to inadequate lymphatic drainage and cause swelling. If someone with lipedema also has lymphatic system dysfunction, they may also present with lymphedema. If they have both conditions together, it is called “Lipo-lymphedema.”
Did You Know?
5-12% of women (approximately 10 to 17 million people in the U.S.) are thought to be impacted by lipedema. The disease crosses demographics like age, race, ethnicity, and education.
Clinical Perspective
Diagnosis and Treatment: The Standard of Care
By Vein Health News Staff
Lipedema is not a rare disorder, but due to lack of research and general awareness, a proper diagnosis is often delayed. Fortunately, recent scientific research and growing patient awareness are helping to increase knowledge of and about the condition.
Diagnosing lipedema
In May 2021, a committee based in the U.S. published a consensus guideline for the standard of care for lipedema. The three key aspects of diagnosis are listening to a patient’s family and medical history, physical examination, and ruling out possible causes of symptoms.
Patient history — Clinicians should complete a detailed history with the patient. Noting such things as:
- Medical history
- Family history of similar body type (to consider heredity)
- Difficulty losing fat in affected areas
- Onset/worsening at time(s) of hormonal change
- Pain, tenderness, heaviness in affected areas
- Tendency to bruise easily
- Decreased functional ability (including mobility)
- Decreased quality of life
- History of joint issues
- Symptoms persist despite: elevation, nutritional interventions, exercise, diuretics, bariatric surgery
Physical Examination — An exam includes visual inspection and physical palpation. (A Stemmer sign test is also recommended to assess for co-morbid lymphedema.) Take into consideration the location and symmetry of adipose tissue.
- Visual Inspection: Bilateral, symmetrical fat accumulation that can appear in a combination of the legs, buttocks, hips, arms and/or lower trunk. Disproportion between upper and lower body. Lobules of fat may present at hips, medial knees, lateral malleoli, or above elbows. Presence of raised ridge/fold of fat, possibly a “cuff” at wrists and ankles.
- Palpation: Presence of nodular and/or fibrotic texture in affected areas. Lipedema tissue texture can vary widely; It may feel like fluffy fat with nodules embedded in it, have a dense, cement-like texture, feel granular or grainy, or even have a spongy texture. Nodules may feel like rice, peas, or walnuts. Fibrosis may feel dense, firm, woody, putty-like, or cement-like.
- Stemmer Sign Test: Lipedema typically spares the hands/feet and presents with a negative Stemmer sign. However, a positive sign does not rule out lipedema but likely indicates the presence of Lymphedema. (If both conditions are present, this is termed “Lipo-Lymphedema.”) Performing the test: pinch the skin on the back of the second toe. If you cannot create a fold of pinched skin, this results in a positive sign for lymphedema. If you can pinch, the Stemmer sign is negative, and lymphedema is likely not present.
Different types and stages of lipedema
Lipedema is divided into five types based on the location of fat deposits, and the different types can overlap.
- Type I: Between the umbilicus and hips/buttocks
- Type II: Between the pelvis and knees
- Type III: Between the pelvis and ankles
- Type IV: Between the shoulders and wrists
- Type V: Between the knees and ankles
Lipedema also has five stages based on the severity of the fatty deposits and problems they cause.
- Stage 1: Skin is smooth but there are pockets of enlarged fat tissue.
- Stage 2: Skin is uneven with indentations and large mounds of fat tissue can be seen and felt.
- Stage 3: Large amounts of fat tissue cause deformation, typically around thighs and knees.
Consider the emotional aspect
Lipedema is a difficult condition to live with. In addition to the physical pain, many women have had to cope with their perceived failure to lose weight by typical methods. This can increase the incidence of depression, anxiety, and/or eating disorders. Therefore, clinicians should offer people with lipedema a mental health consultation as part of their treatment, especially when there are signs or symptoms of the negative emotional impact of lipedema. Improving one’s mental health has been proven to increase self-care by women with lipedema.
Management
Living with Lipedema: Effective Management and Care
By Benjamin Lee
Lipedema is a complex condition. While there is not yet a cure for lipedema, there are an array of treatment options that can help patients manage their symptoms and improve their quality of life. According to Robin Dobrinick, Nurse Practitioner at the Vein Healthcare Center, taking a multimodal approach is the most effective. "We recommend that patients employ a variety of treatment modalities, starting with conservative and minimally invasive management strategies before considering surgical intervention," said Dobrinick.
Compression
Graduated compression therapy is essential for managing lipedema symptoms and is considered a first-line intervention. Compression improves mobility, reduces pain and swelling, and improves limb shape and comfort.
Nutrition
Even though lipedema fat is resistant to weight loss from dieting or even bariatric surgery, what one eats is still an important component of treatment. The dietary guidelines that yield the best results are anti-inflammatory, such as ketogenic or low-carbohydrate diets.
MLD Therapy
Manual Lymphatic Drainage (MLD) is a specific, gentle massage technique to stimulate the lymphatic system and move fluid out of affected tissues. Better lymphatic flow can improve limb function and overall mobility.
Exercise
Moving the body is essential for managing lipedema symptoms. Exercise also helps the lymphatic fluid move through the lymph system. Pain from lipedema can make exercise challenging, so try low-impact activities like swimming, water aerobics, walking, and moderate stretching.
Pain management and medication
Certain medications, both prescription and over the counter, may decrease swelling or inflammation, or provide relief from pain. These include GLP-1 and GIP agonists, Stimulant medication, Metformin, Ketoprofen, Diosmin MPFF, and Turmeric/Curcumin. Patients should discuss any medications or supplements with their primary care physician.
Surgical interventions
The three most studied surgical techniques to remove lipedema tissue are tumescent liposuction, water-assisted liposuction, and power-assisted liposuction. All three depend on the tumescent technique, which involves introducing large volumes of solution into the fat below the skin space in order to swell (tumesce) the area. According to leading liposuction specialist Dr. Thomas Wright, MD, FAVLS, RVT, some surgeons will not operate unless a patient first establishes healthy routines with conservative treatments and adheres to compression therapy and dietary guidelines.
Mental health and wellbeing
In addition to physical symptoms, lipedema can affect a person’s mental health and quality of life. In fact, there is a high prevalence of depression and other mental disorders in patients with lipedema. This can lead to low energy, feelings of hopelessness, low self-esteem, or eating disorders. Emotional, psychological, and social wellbeing are key aspects of overall health, so counseling may be worth considering, depending on the patient.
Q&A with Dr. Thomas Wright
Dr. Thomas Wright, MD, FAVLS, RVT, is the medical director of Laser Lipo and Vein Center in St. Louis, Missouri. Dr. Wright has been treating patients with lipedema for more than 20 years and has a deep understanding of the disease.
Why do patients with lipedema seek a surgical solution?
The simplest reason is having lipedema symptoms or morbidity from lipedema that is not fully managed with non-surgical means. A modified type of liposuction can reduce bulk tissue which can aid in mobility, knee function, and joint mechanics.
What steps would you recommend before surgery?
Lipedema needs to be treated comprehensively, including an anti-inflammatory diet and daily wearing of medical grade compression. It’s important that these non-surgical treatments are implemented before surgery, when their effects can be fully appreciated.
What are the success rates of lipedema surgery?
The randomized controlled study of lipedema surgery, called the LIP LEG study, showed over 70% of women with lipedema who underwent lipedema liposuction had significant improvement in pain and quality of life versus 10% of women in the conservative control group. The results of this study show a 26:1 odds ratio of significant improvement for those who had surgery.
Is liposuction a cure for lipedema?
Lipedema surgery is not a cure for lipedema. It can improve mobility, reduce pain, and increase quality of life, but it can only reduce the lipedema tissue; some fat tissue will remain. Lipedema must be treated comprehensively with lifelong adherence to diet and other lifestyle changes.