Cover Story
Standing on the Job: How At-Risk Occupations Put a Strain on Veins
By Jennifer Boggs | Feature
Nurses and doctors. Teachers, hairdressers, and food servers, not to mention, bank tellers, assembly line workers, toll collectors, pharmacists – there are many occupations where people are on their feet for hours on end.
These jobs often take a physical toll, especially on the legs and feet. One reason for discomfort in the lower extremities is poor circulation, but what exactly does that mean? The major parts of the circulatory system (also known as the cardiovascular system) are the heart, arteries and veins. The heart pumps blood to the arteries, which take the oxygenated blood to all parts of the body. Healthy veins carry deoxygenated blood back up to the heart, the "muscle pumps" in our feet and calves helping the blood to travel against gravity.
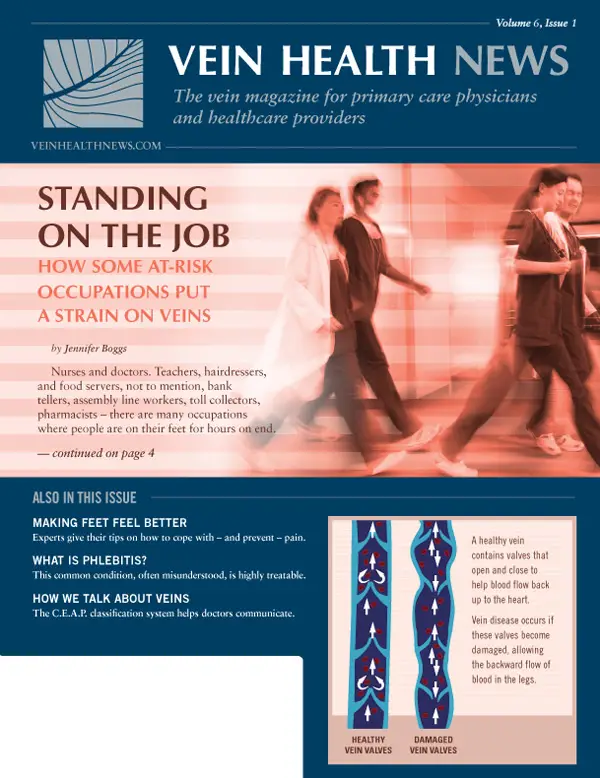
If you are standing on your feet all day, your circulatory system isn't working as efficiently as it should. And if you have venous (vein) issues, the problem can be exacerbated. In leg veins, there are valves that open to allow the blood to flow one way: up. If the valves in the veins become damaged, some blood will flow back into the legs or feet and "pool" there resulting in a feeling of heaviness, leg pain, varicose veins, or other symptoms. This is sometimes referred to as venous congestion or reflux.
Recognizing the symptoms
Expert Tips for Legs and Feet
-
Kenny Maisak, DPM: "Get supportive shoes with a solid heel counter and laces... avoid the impulse to get a soft or cushioned shoe."
-
Chris Stanley, Pedorthist: "About 80% of Americans are wearing shoes that don't fit correctly... When shopping for work shoes, shop at a shoe store that measures feet."
-
Tom Musone, Juzo: "Wearing compression every day can prevent edema... make sure you wear graduated compression stockings."
-
Ginger LeClair, Nail Tech: "Use a pumice block when you shower to clean away any dead or rough skin on the heels. Apply a foot cream at night."
Karen Bragdon, 53, is a Physical Therapist and Orthopedic Certified Specialist at York Hospital in Wells, Maine. Her tasks vary depending on her caseload, but on average she's on her feet 80% of the day. At first Bragdon noticed "very unsightly bulging veins" in her legs, behind the knees, and at the ankles. But there were other symptoms showing up that she did not realize were warning signs of venous disease. By the end of the workday her feet and legs would be extremely tired and, many times, swollen. She also began having leg cramps at night.
A runner, she also realized that running wasn't feeling as good as it used to, either during or afterward. Bragdon's leg problems – both visible and not-so-obvious – gradually became worse until a new condition presented itself, one she affectionately named "twitchy legs." "I started having this annoying thing happen more and more where I constantly had to fidget," she said. "I could not stop moving my legs, even when I was just sitting on the couch watching TV."
Bragdon didn't put all the pieces together until she was talking to one of her patients who had also experienced symptoms before she sought vein treatment. After an a-ha moment, Bragdon made an appointment for a consultation with a Board certified phlebologist. A diagnostic ultrasound confirmed venous reflux; the vein valves in both legs were not functioning properly, her left leg worse than the right leg.
The treatment plan included endovenous laser ablation (EVLA) to fix the reflux on Bragdon's left leg and ultrasound-guided sclerotherapy to treat the source of the dysfunctional vein valve on the right leg. She described both procedures as "a piece of cake." Four months later and the leg twitching and nighttime cramping are 90% gone as Bragdon's stamina at work continues to improve.
"I would encourage anyone to get a consult if they're having any questions about possible symptoms or chronic issues with their legs," said Bragdon. "The biggest surprise to me was that all of those things that I was feeling could be caused by veins."
Recent research
Bragdon's experience is far from unique. Several studies in the past five years have attempted to investigate the prevalence of varicose veins among professionals who work long hours on their feet. In 2015, research reported in the International Journal of Nursing Practice looked at the relationship between the occupational and demographic hazards that characterize varicose veins and their intensity among nurses.
A cross-sectional study carried out among 203 nurses from three hospitals in Amol, Iran found that the prevalence of varicose veins (of varying degrees) was 72.4%, with women having a higher prevalence compared with men, 77.9% vs. 56.9%. According to the study, a patient's occupation can be among the factors that intensify vein disorders. Blood hydrostatic force in standing position along with other intrinsic factors such as heredity can contribute to varicose creation because upwards blood pumping takes place with muscle contraction. Standing is worse than walking for varicose patients and hydrodynamics pressure does not help blood discharge in this state.
A study conducted in southern Taiwan aimed to evaluate whether prolonged standing at work can increase the risk of developing varicose veins. "Varicose veins in hairdressers and associated risk factors: a cross-sectional study" recruited 182 hairdressers in southern Taiwan to participate in a survey. The researchers concluded that in hairdressers 45 years old or younger, family history of varicose veins is a major risk factor for developing lower limb varicose veins, while in those who are older than 45, the effects of occupational risk factors are more prominent.
From one physician to another
Dr. Michael Enns sees many patients at his vein practice who are nurses and pharmacists. When Dr. Enns first started treating veins, however, he didn't realize how personal the issue of venous disease was to him. "My whole family has the worst veins, so I got used to seeing varicose veins," said Dr. Enns. "My mom's veins were so bad, I thought it was normal to elevate your legs on the back of the couch twice a day."
Dr. Enns himself had experienced leg pain for more than five years (prior to treating veins), so much so that the pain would wake him up at night and he'd have to take ibuprofen and stretch his legs. Eventually, he began to see skin changes on both of his shins. His legs itched and continued to ache, but his dermatologist didn't recognize it as a venous issue. She gave him a topical steroidal cream, but the skin changes gradually worsened.
At the height of his leg distress, Dr. Enns started working at a vein care clinic and began to understand the misconceptions he had about varicose veins, including the erroneous belief that vein treatment is only cosmetic. As he learned more and listened to patients, he realized his leg issues might all stem from venous insufficiency. Dr. Enns has now had his own practice for four years, the Central Arkansas Vein Center in Little Rock. He has worn compression every day for years and recently underwent Endovascular Radio Frequency therapy.
He admits that "physicians and pharmacists are the worst patients because they think they already know everything," but because the field of phlebology (vein health and treatment) is relatively new, many healthcare professionals don't have the latest knowledge to diagnose and treat vein disease.
Dr. Enns's approach to physician education is to focus on skin changes and leg sensation. He encourages his primary care colleagues to refer patients to him if there is any skin discoloration, psoriasis or rash below the knees, or any leg swelling, itching, discomfort, or restlessness in the legs. Like his own experience of being prescribed steroidal cream for his apparent leg rash, Dr. Enns knows that you can treat the symptom without treating the cause.
If patients complain of leg achiness or fatigue but don't present with visible symptoms, Dr. Enns will look for other clues. One of the first things he looks for is whether patients are taking a diuretic for swelling in the ankles or medication for restless legs. Medications for neuropathy may also be an indication of undiagnosed venous problems.
Dr. Enns's number one suggestion for people on their legs all day is to wear a good, trusted brand of graduation compression stocking. In addition to preventing leg swelling and fatigue, wearing compression can also be a good diagnostic tool. When Dr. Enns began to wear them, the discoloration and itching on his shins went away. If the compression makes a profound difference, it may be aiding a "hidden" venous issue, one that could be very treatable.
Facts & Fallacies
Phlebitis: Facts & Fallacies
By Benjamin Lee
Imagine a whitewater river. It might be fast or slow moving, but no matter the speed of the river, the water travels smoothly because it's all flowing in one direction. Now imagine a place in the river where it starts to bend. It's at this juncture that the water becomes turbulent because liquid can't change direction smoothly. The swirling reverse-current that is created is known as an eddy.
What does this have to do with veins? When the blood is flowing up the leg in a vein, and then – due to venous reflux – it turns and starts going back down toward the feet in a vein, "eddies" are created at the intersection of the deep vein and the superficial vein. Phlebitis almost always starts at a juncture where there's turbulence.
Phlebitis describes a condition in which a vein in the superficial vein system becomes inflamed and swollen. (It is also referred to as superficial phlebitis.) Spontaneous phlebitis happens when there is a sudden onset of vein inflammation.
Three out of 10 patients may develop spontaneous phlebitis after endovenous laser ablation (EVLA) therapy, but according to phlebologist (vein specialist) Cindy Asbjornsen, D.O., ABPh, it is very preventable. "We rarely see phlebitis post procedure at our vein care practice, especially if patients follow the post-procedure guidelines closely," said Dr. Asbjornsen. Post-operative requirements include wearing prescribed graduated compression stockings and walking at least 30 minutes a day.
If phlebitis does occur and is not treated in its early stages, thrombophlebitis, or the formation of a blood clot associated with phlebitis, can develop. Think back to the whitewater river analogy: at the critical junctions where there is lots of turbulence, the blood in the center of the "eddy" is staying still – and any time blood stays still, there is a risk for clotting. If a patient does not experience pain or swelling, heat, or she should apply heat to the area, elevate the legs, and take a nonsteroidal anti-inflammatory drugs, such as ibuprofen or naproxen.
The right diagnosis and treatment
Anyone with venous dysfunction can get phlebitis or thrombophlebitis, and both are very common, but historically the medical community has received little training about these conditions and how to treat them. Some physicians underestimate how much a patient with thrombophlebitis can suffer, even though the pain can be incapacitating. "I've seen patients with veins that are rock hard and feel extremely tender; some have had to stay home from work it hurts so badly," said Dr. Asbjornsen.
She emphasizes that although untreated phlebitis can present very dramatically, early and aggressive care can "nip it in the bud." While many physicians have been trained to treat phlebitis with antibiotics or anti-coagulation, the proper treatment for phlebitis is usually to apply heat (NEVER ice) to the area, elevate the legs, and non-steroidal anti-inflammatory medicine.
Before ultrasound, all phlebitis was treated as septic phlebitis (caused by bacteria in the venous system) and the treatment was a course of antibiotics. Dr. Asbjornsen only prescribes antibiotics if someone has a fever that is 100-degrees or higher (an indication that it the phlebitis might be septic in origin). The only time that anti-coagulation is appropriate is when the thrombophlebitis is within at least two centimeters from the saphenofemoral junction (where the great saphenous vein in the superficial vein system enters the deep vein system).
What about DVT?
To review, phlebitis (also known as superficial phlebitis) is the inflammation of a vein. Symptoms include redness, swelling, tenderness, and pain in or along a vein. Thrombophlebitis is a blood clot in the superficial vein system. Deep vein thrombosis (DVT) is a blood clot that forms in the deep vein system.
Superficial phlebitis should not be mistaken for a DVT, because with phlebitis, you can almost always see the vein that is involved. Phlebitis often presents like a big, red streak and usually comes with symptoms, whereas DVT sometimes presents with no symptoms.
If phlebitis is located on the high thigh, however, the patient should get an ultrasound to make sure that the deep vein system is not involved, or the vein involved is >2 centimeters from any deep connection. It's important to note that it is possible for a blood clot in the superficial vein system to grow into the deep vein system. A 2006 study in the Journal of Family Practice found that the condition confers a 10-fold risk of developing DVT within six months compared with controls – but that absolute risk of DVT following SVTP is just 2.7%, and "watchful waiting is probably a reasonable approach in primary care."
Preventing phlebitis
Dr. Asbjornsen advises that “all the things that prevent DVT” also keep phlebitis at bay, including evaluation by a board certified phlebologist if venous disease symptoms are present in the legs: spider veins, varicose veins, heaviness, achiness, and/or discoloration or changes of the skin.
Also, stay adequately hydrated and stay active to promote circulation. Avoid prolonged periods of inactivity (such as after surgery or long stretches of sitting). Last, but not least, maintain a healthy weight, eat a healthy diet, and don’t smoke.
Some doctors recommend an anti-inflammatory diet, such as the DASH diet (dietary approaches to stop hypertension). Supplements such as fish oil, horse chestnut seed extract, ginger, and tumeric are natural anti-inflammatory agents.
Resources
Van H. Weert, MD, PhD. Spontaneous superficial venous thrombophlebitis: Does it increase risk for thromboembolism? J Fam Pract. 2006 January;55(1):52-57
TIPS FOR PREVENTING PHLEBITIS
- Stay active to promote circulation
- Avoid prolonged periods of inactivity (such as after surgery or long stretches of sitting)
- Stay adequately hydrated
- Maintain a healthy weight
- Eat healthy foods; consider an anti-inflammatory diet, such as the DASH (Dietary Approaches to Stop Hypertension) approach
- Don't smoke
- Seek evaluation by a board certified phlebologist if venous disease symptoms are present in the legs: spider veins, varicose veins, heaviness, achiness, and/or discoloration or changes of the skin
Classification
C.E.A.P. - Communicating Vein Severity
By Vein Health News Staff
Venous insufficiency is a progressive disease. Without intervention, the severity of symptoms will increase and complications may arise that can have a serious impact on overall health. In order to have a standard way to talk about vein problems, a group of experts created a classification system known as C.E.A.P.: Clinical + Etiology + Anatomy + Pathophysiology. The "C" in C.E.A.P. stands for the clinical severity rating of a patient's veins and is the most significant in physician-to-physician communication. For patients, recognizing what C.E.A.P. classification they are in may help them to decide if and when to seek treatment.
STAGE 1: Spider Veins
C1 refers to patients with telangiectasies (spider) and/or reticular veins. Treatment of spider veins can help to slow or halt the progression of venous disease early and at its source.
STAGE 2: Varicose Veins
C2 describes patient with vein diameter that is larger than 3-4mm; the veins are pressurized enough to rise up off the skin. If the varicose veins are tense and bulging when the patient stands, then become less so when the leg is elevated, then it is likely a superficial vein issue and easily treatable.
STAGE 3: Edema without Skin Changes
C3 is swelling related to venous disease, often below the knee. Best visualized from the back than the front, diagnosis of C3 can be tricky. Only a valve study ultrasound can confirm edema is caused by venous disease, and sometimes the only symptom is swelling but no visible veins.
STAGE 4: Skin Discoloration
C4a, b refers to a variety of skin changes. C4a: corona phlebectasia (blue pigmentation and eczema). C4b: lipodermatosclerosis (hardening of soft tissues) with hemosiderin staining, or atrophie blanche (whitish skin area that looks like scar tissue and can be mistaken for a healed ulcer). C4 skin damage almost always occurs on the the lower leg at the "gaiter area."
STAGE 5: Skin Changes with Healed Ulceration
C5 is a healed skin ulcer. (One of the shortcomings of CEAP scale is once a C6, a patient can never do better than a C5.) A healed venous leg ulcer is highly likely to recur if the underlying vein problem has not been treated.
STAGE 6: Skin Changes with Active Ulceration
C6 is an open active ulcer and the most severe category. The ulcer is an open sore with no skin covering the underlying tissue; it can appear pink with granulation tissue, or it can have yellow exudate. The surrounding skin is usually red as the body is using inflammation to try to heal the ulcer.
Patient Perspective
One Patient's Perspective: Success the Second Time
By Benjamin Lee
Twenty-seven years ago, Shelly Rinfret got her veins "done." After the birth of her second child, the varicose veins on her legs had become so pronounced that she sought medical treatment, which, in those days, meant vein stripping and ligation. The surgery worked to reduce the bulging veins in Shelly's legs – at least for a while.
Shelly, 55, has had to contend with vein issues for most of her life. Her maternal grandmother had them, and she remembers seeing the start of varicose veins on her own legs even as a teenager. Unfortunately, Shelly developed more varicose veins several years after her initial vein stripping.
She has been a registered nurse at Southern Maine Healthcare for 18 years, and working in the same day surgery/post anesthesia care unit, she spends most of her long days on her feet. In addition to her bulging veins, she started becoming concerned about symptoms such as achiness and a feeling of heaviness in her legs.
It wasn't until a co-worker developed a venous stasis ulcer from one of her varicose veins that Shelly decided to seek professional help a second time. "I took another look at my legs and thought, maybe I should go see someone again," she said. "I wanted relief, but I also wanted to know if I was at risk for ulcers."
Shelly's legs needed a lot of attention, and for her the results have not come overnight. Over three years of seeing a board certified phlebologist, Shelly has had two endovenous laser ablation (EVLA) treatments to one leg, one EVLA treatment on the other leg, plus several sessions of sclerotherapy on both legs.
As a healthcare professional, it was important to Shelly to go to a doctor for whom vein treatment is a priority, rather than someone who "does veins on the side." Moreover, she has referred several patients to her vein specialist – all of them nurses!
Now after various phases of treatment, Shelly says that her legs feel "really good," even after nine hours on duty at the hospital. Knee-high compression stockings with a gradient of 30-40mmHg also help to improve circulation and prevent leg fatigue. According to Shelly, the biggest takeaway from her experience is to investigate the problem before you get varicose veins, in many cases the "end product" of a faulty venous system.
"Back when I got my veins stripped, there were limited solutions, but now with ultrasound, doctors can tell much better where there's a deeper problem," she said. "Now I would tell anyone: don't wait until you have legs full of varicosity on the outside; if you're starting to see symptoms, go see what the issue is before it gets to that stage."
Concerned about your vein health?
Contact the Vein Healthcare Center for an evaluation.
Contact Us