Cover Story
Veins and Feet: A Direct Connection
By Jennifer Boggs | Feature
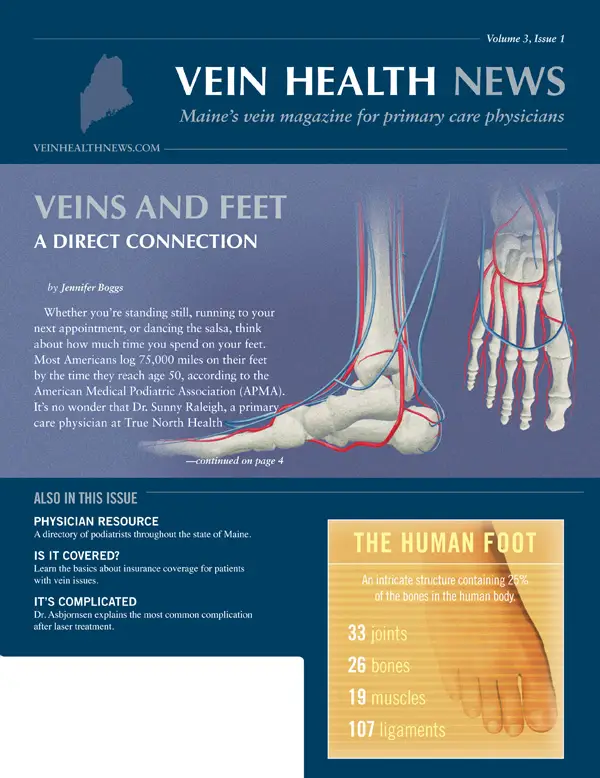
Whether you're standing still, running to your next appointment, or dancing the salsa, think about how much time you spend on your feet. Most Americans log 75,000 miles on their feet by the time they reach age 50, according to the American Medical Podiatric Association (APMA).
It's no wonder that Dr. Sunny Raleigh, a primary care physician at True North Health Center in Falmouth, Maine, says that feet are a vital component to overall health. "From an osteopathic perspective, we see the feet as our foundation," said Dr. Raleigh. "When you consider and examine the feet, you can usually unwind many physiological concerns in the rest of the body."
The fascial, musculoskeletal, nervous, lymphatic, and venous systems in the feet all have intimate feedback connections to the rest of the body, so paying attention to patients' feet allows Dr. Raleigh to "see the whole person" and assess if something else may be contributing to a problem. She emphasizes the importance of addressing, not just the physical manifestations or symptoms, but also the underlying issues. Her approach is to look upstream for the causes of the downstream diagnosis, continually seeking answers to the question: what is the systemic breakdown that we need to try to repair?
When examining a patient's feet, she looks for skin breakdown, toenail fungus, swollen ankles, discoloration of the toes, as well as sensations at the bottom of the feet (the latter in diabetics, especially). She says that checking a patient's pedal pulses is vital to test blood pressure at the foot. In addition to a thorough physical exam, Dr. Raleigh will listen to each patient's medical story as a way to begin to hone in on the potential culprits behind any suspected disease. Treating venous reflux can often improve foot-related problems.
Dr. Kenny Maisak, a Doctor of Podiatric Medicine (DPM) at Portland Foot & Ankle in Portland, Maine, also sees every day how health issues can manifest in the foot. He describes it as a "closed kinetic chain," meaning the motion of the foot directly relates to the motion of the ankle, knee, hip and back. For example, if a patient is favoring one foot, it may be due to a pinched nerve in the lower back. Likewise, if a patient is having foot issues, it may contribute to, or even create, knee, hip or back problems.
Veins and feet
Problems in the feet can be manifestations of arterial or venous concerns. Peripheral arterial disease (PAD) and other related disorders are important to consider when examining the foot. However, the close correlations between foot issues and venous disease—the impairment of blood flow back up towards the heart—also deserve attention. If venous return is impeded due to damaged valves in the venous system, then the backward flow of blood can pool in the legs and feet. The vein insufficiency, or venous reflux, can cause leg pain and fatigue, spider veins or varicose veins. If left untreated, it can lead to edema, corona phlebectasia and, ultimately, ulcers.
Predominantly, most vein issues will present in the medial ankle or anterior shin area. If veins aren't functioning properly, then edema will often occur. Edema is the venous symptom that Dr. Maisak encounters most. He said that people with mild edema in their feet and legs don't always realize it, but over the years it can create chronic reactions in the skin, such as hemosiderin staining, which is a brown or rusty discoloration of the lower legs. (When vein valves fail, regurgitated blood forces red blood cells out of capillaries; those dead cells then release iron, which gets stored in tissues as hemosiderin.)
The onset of edema can be a prelude to other, more serious issues, as the skin becomes susceptible to breakdown and venous ulceration. "Venous ulcers are always very challenging, and sometimes impossible, to heal," said Dr. Maisak. "Early detection and control of edema will reduce those chronic changes of the skin, greatly lowering the risk of long-term effects."
According to Dr. Dwight Blease of Casco Bay Podiatry in Brunswick, Maine, some of those long-term effects may include bacterial skin infection or infection of the bone, as well as "all the morbidity associated with those conditions." There are a number of minimally invasive treatments of venous disease available, including endovenous laser ablation (EVLA) and sclerotherapy. Dr. Raleigh suggests that there may also be a role for osteopathic manipulative medicine in treating vascular and venous insufficiency. A 2012 study showed that adding myofascial manipulation to venous treatment increased venous return in post-menopausal women (when compared to direct venous treatment alone).
Making the connection
Because the primary care physician is typically the first encounter a patient with complaints around venous disease and related diseases will have, that initial contact can set the stage for a treatment plan. According to Dr. Raleigh, a good diagnostic exam often leads to a referral for further studies and intimate care with specialists: "We all have our role to play in supporting the overall health of each patient, with the PCP acting as QB, making sure the plays are going off as desired. It's our priority to make sure that the patient is getting the best possible care by using specialists and adjunct providers optimally."
Dr. Blease has been practicing podiatry for more than 25 years. He explains that when he was in podiatry school there was an emphasis on the arterial system, with little study of the venous system. He also recalls having a patient who was told she could never have surgery done on her foot because she'd had her veins stripped and the potential for severe swelling and delayed healing were too great. "Now with these newer techniques in vein treatment, our patients heal quicker and we get an improved functional result," Dr. Blease said. "We can see how phlebologists' skills and expertise can help us do our job better."
Dr. Maisak concurs. If he sees that a patient has venous insufficiency, he will consult a vein specialist for possible treatment. Vein insufficiency (often accompanied by edema) may be a contraindication to surgery, because of the likelihood that the skin will have trouble healing. He also recognizes that podiatrists can play a role in early detection for venous or vascular issues. "We see a lot of lower extremities, so we can be a good source for identifying vein-related problems," said Dr. Maisak.
Even the APMA, the leading professional organization for podiatrists in the U.S., has acknowledged the link between podiatry and phlebology. In 2013, the APMA joined the "Rethink Varicose Veins" campaign to raise awareness of venous disease diagnosis and treatment. Dr. Blease sees the "Rethink" campaign as a step in the right direction. He believes this is an issue that goes undiagnosed and untreated in many situations, and he encourages all physicians to learn more about it: "We all share the same goal—keeping our patients active, independent, working and enjoying their favorite things in life."
FOOTNOTES
- Ramos-González E, Moreno-Lorenzo C, et al. Comparative study on the effectiveness of myofascial release manual therapy and physical therapy for venous insufficiency in postmenopausal women. Complement Ther Med. 2012 Oct 20(5):291-298.
Awareness
Olympian Champions Vein Health
By Vein Health News Staff
At the 1992 Summer Olympics, swimming legend Summer Sanders won two gold medals, one silver and a bronze for the U.S. swim team. Years later, after the birth of her second child, this healthy, active athlete developed varicose veins—a precursor to chronic venous insufficiency (CVI). Fast-forward to 2012. Sanders has had her veins successfully treated and her legs no longer feel "achy and heavy, especially after a long day."
She is now the national spokesperson for Rethink Varicose Veins, an educational campaign that encourages those suffering from varicose veins to learn more about their condition and to speak with a vein specialist about treatment options. The campaign started as a joint effort of the American College of Phlebology (ACP), Society for Vascular Surgery (SVS) and American Venous Forum (AVF). This year, the American Podiatric Medical Association (APMA) joined the coalition. In fact, Sanders helped open the 2013 APMA Annual Scientific Meeting in July.
Dr. Joseph Caporusso, DPM and immediate past president of APMA, found Sanders' story to be "enlightening, and even inspirational." "Podiatrists play a role in keeping America walking, and venous disease is a common component of that," he said. For Dr. Caporusso, the venous-related conditions he encounters most often are varicose veins, which affect the feet and ankles, and ulcerations, usually on the inside ankle toward the midline of the body. He says that podiatrists also have patients with unexplained calf pain; they must determine whether the patient has a Deep Vein Thrombosis (DVT), which could be life-threatening.
More than 30 million Americans suffer from vein disease each year, but less than 10% seek treatment. Efforts like Rethink Varicose Veins can go far in educating the public that venous disease is a health concern worthy of diagnosis and treatment, especially when different medical professionals take a team approach toward patient care. "Many of our colleagues work with vein specialists and vascular surgeons, and our partnership with this campaign allows us to go even further," said Dr. Caporusso.
Insurance
A Primer on Billing in Phlebology
By AJ Riviezzo
"Will my insurance cover this?" This is a commonly asked question by patients who are interested in pursuing vein treatment. The short answer is: yes. Most insurance plans—including Medicare—do cover the primary treatment (endovenous laser ablation, or EVLA), along with the various attendant services, such as ultrasounds and sclerotherapy (an injection of a sclerosing solution into a problematic vein).
The longer answer is: it depends on the insurance plan and the patient's prescribed treatment. The patient must meet the medical necessity thresholds established by his or her insurance plan. Common guidelines that demonstrate symptomatic venous reflux include: the impact of the disease on the patient's activities of daily living, the size of the vein to be treated, and the presence of venous reflux.
For most vein patients, their first visit to a phlebologist (vein specialist) will be a consultation appointment, where the doctor conducts a physical examination of the legs (including an ultrasound scan), reviews the patient's health history, and discusses diagnosis and treatment options. Generally, this appointment is billed to the patient's insurance and the cost is typically the co-pay for a doctor's office visit. If a patient has symptoms of venous disease, there is usually one other criterion that must be satisfied before coverage is approved. Most carriers require a period (6-12 weeks) of wearing graduated compression stockings before providing coverage for varicose vein procedures. The stated reason for a trial of conservative treatment (which includes the wearing of compression stockings) is to ensure that non-surgical remedies are tried and fail prior to approving surgical treatment.
It should be noted that there is a difference between "cosmetic" sclerotherapy and "medically necessary" sclerotherapy. So-called cosmetic sclerotherapy, which is not covered by insurance, is for the removal of the small spider veins. Medically necessary sclerotherapy, which is typically covered by insurance, is for the destruction of symptomatic veins that typically have to meet a diameter requirement.
Most office staffs at vein care offices work directly with the patient's insurance carrier to obtain approval or authorization for the patient's venous treatment. The staff will commonly submit the results from the diagnostic ultrasound, along with a copy of the patient's history and a Physical and Letter of Medical Necessity. That said, patients can always check with their individual insurance companies to determine which treatment options are covered. (Some insurance policies even pay for "durable medical goods," including graduated compression stockings.) It's to the patient's benefit to be educated about his or her insurance policy, co-payments, and deductibles.
Primary care physicians can also help patients with insurance reimbursement or approval. If the patient is complaining of leg pain, swelling, and other symptoms, placing the patient in good compression stockings and prescribing NSAIDs is a great first step in the process. If a claim is denied, the specialist's office, and/or the patient, can review the explanation of benefits (EOB) to learn the reason for the denial. If the EOB does not explain the reason for denial, they can contact the claims department and request an explanation. In addition, all insurance carriers have an appeals process.
On October 1, 2014, the ICD-9 (International Classification of Diseases 9th Edition) code sets used to report medical diagnoses and inpatient procedures will be replaced by ICD-10 code sets. ICD-10 will affect diagnosis and inpatient procedure coding for everyone covered by Health Insurance Portability Accountability Act (HIPAA), not just those who submit Medicare or Medicaid claims. And although it will impact the entire physician community regardless of specialty, phlebology treatments and processes will likely not change at all.
FAVQ
Frequently Asked Vein Questions
By Dr. Cindy Asbjornsen
Can a patient receive vein treatment if he or she is on blood thinners or chronic pain medications?
Yes, a patient can be treated for venous issues when taking either blood thinners or chronic pain medications. In fact, for patients who take these types of medications, treating their veins is not only possible, but can even be advantageous. Although blood thinners can be a relative contraindication in some of the more invasive procedures where hematomas may be a potential complication, most venous procedures are performed with nothing more than a 22-gauge needle stick, thus if a patient is on blood thinners, it is not an issue at all. I always warn my patients on blood thinners that they may be more prone to post-op bruising, but aside from that, there is really no difference.
As for chronic pain medications, this should have no bearing at all on vein procedures. In many cases, patients who are prescribed pain medication for leg pain are able to cease taking their chronic pain medications after their venous issues have been resolved. My standard protocol is to offer patients a muscle relaxant and/or a mild narcotic pre-op—not because the procedure itself is painful, but because the time spent lying on the exam table may cause a strain on their neck or back. Every patient is different in this regard, and we offer pillows, blankets and hot packs to make the experience as comfortable as possible, whether the patient opts for pain medication or not. Of course, patients should always tell their physician and medical care team about any medications that he or she is taking.
What is the most common complication or side effect after an EVLA procedure?
The most common complication after endovenous laser ablation (EVLA) is bruising and swelling of the treated area. Both bruising and swelling are self-limited and usually resolve within the first two weeks following the procedure. Phlebitis is another common adverse complication, however phlebitis can occur with any IV stick, or even spontaneously from varicose veins. It is more common with EVLA because with this procedure, we are intentionally irritating the vein wall. The national incidence for resulting phlebitis is recorded at ~30%, however, at my office, we instruct patients who experience any post-operative pain to use elevation, heat and non-steroidal anti-inflammatory medications, essentially treating pain prophylactically. Thus, we have a much lower incidence. People with dilated veins are at a greater risk of developing phlebitis.
The complications that follow EVLA are few, and it's worth noting that because venous disease is a progressive disease, its symptoms intensify over time. Without treatment, early symptoms of venous disease can lead to lipodermosclerosis, a disease of the skin and connective tissue; an increased chance of superficial venous thrombophlebitis, clotting in the superficial veins that causes severe pain and incapacitation; spontaneous bleeding of an exposed or injured vein; and ulceration, wounds on the leg that will not heal.
Patient Perspective
One Patient's Perspective: Positive Side Effects
By Benjamin Lee
Gary Stewart did not go to a vein specialist because his legs hurt, or to fix his foot issues, or even for cosmetic reasons. After being evaluated and treated by a vein specialist, however, both leg and foot problems were resolved—and his bumpy veins have disappeared, an unexpected side effect.
It all started when the 60-year-old engineering supervisor went to his family doctor for an annual physical. Stewart had no leg pain, but the visible varicose veins on his legs gave him cause for concern. "For me it was all about prevention," he said. "I wanted to make sure that my legs were healthy."
Stewart's doctor referred him to a board-certified phlebologist who gave him a full venous evaluation, which included a physical exam and diagnostic ultrasound. The vein specialist also collected a complete health history—and took note that both of Stewart's parents had varicose veins, though they never sought treatment. (Significant research with gene mapping shows that there is a strong link between heredity and venous disease.)
In addition to varicose veins, Stewart had been experiencing what he described as "a fair amount of trouble with both feet." He suffered from plantar fasciitis, a common cause of heel pain, and Achilles tendinitis, a common condition that causes pain along the back of the leg near the heel. For the plantar fasciitis, he had been seeing a podiatrist annually for five years to get cortisone shots on the bottom of his feet. There were no effective treatments available for the tendinitis.
The phlebologist suspected that the build-up of fluid in his feet was the result of poor venous return. In other words, his veins weren't doing an adequate job of getting the blood from his feet to go up through his legs and back to his heart. In December 2012, Stewart had endovenous laser ablation (EVLA) performed on both legs. In the months that followed, he was surprised to see that not only had his varicose veins diminished, but also that the pain in his feet were gone.
"Fixing my foot problems wasn't the goal, but it's good when you fix one thing and the side benefit is you fix something else at the same time." Stewart admits that since the EVLA procedure, he's been "playing a bit more golf" than usual. He also enjoys walking and has had no complaints about his feet. Although he's not sure if he'll experience foot issues in the future, he admitted, "the prospects look good." His goal is to retire in a few years, and preventative care helps increase the odds that his body will be in "relatively decent shape" when retirement comes.
Most vein patients seek treatment when they're experiencing leg pain, swelling, or other symptoms. For Stewart, it was a matter of maintaining his general health. And he wasn't shy about bringing up the issue with his primary care doctor either. "I think patients should be proactive with their health," said Stewart. "If they have any concerns regarding anything, they should discuss it with their family doctor—and get answers to their questions!"
Vein Tech
ScleroTrainer
By Benjamin Lee
Light-assisted or visual sclerotherapy is used to treat "spider veins," or clusters of tiny blue and red veins on the surface of the skin, often resembling bruises. Small needles (usually 32g) provide access to the vein so a sclerosing agent can be injected into the vein's interior wall. This substance causes the vein to become sticky and seal shut, allowing it to disappear. Blood then finds a healthy path back to the heart. There is little risk of complication, and patients often experience an immediate relief of symptoms.
The ScleroTrainer is a product that allows physicians, nurses and other physician extenders to practice their sclerotherapy skills on an artificial model rather than on a real patient. It mimics the feel and visual effect of injecting fluid into reticular and telangiectatic veins. Dvora Nelson, MD, RVT, RPVI and president and CEO of Nelson Medical Enterprises LLC, invented the ScleroTrainer out of necessity.
In early 2011, Dr. Nelson's vein practice was growing rapidly—and so was the wait time for patients. It was taking up to six weeks for new patients to get in to see her, a delay she considered "unacceptable." Eventually Dr. Nelson realized that if she trained someone on her staff to do the sclerotherapy procedure, then she would have more time to "do the things only a doctor can do."
The model is a custom molded "pad of skin" made of visco-elastic polymer. The "veins" range in size from 0.2 to 0.5 mm in diameter and are made of a self-sealing, silicon product. The fluid that simulates the sclerosing agent is actually colored fluid in packets. By adding the right amount of water, it creates a viscosity similar to the real thing. If successfully injected, the fluid goes into an attached balloon that collects it for re-use. The ScleroTrainer also comes with an instructional DVD.
"I wanted to train my RN to do sclero, but she was so nervous about it that she quit," recalled Dr. Nelson. "That's when I knew I needed something I could train people on, but nothing like that existed." Part of the problem, according to Dr. Nelson, is that there is a steep learning curve with significant risks. The clinician is injecting a caustic medication designed to essentially destroy the vein. If he or she injects the skin instead of the intended vein, it could create an ulcer and possibly damage the skin. Hands-on practice with the ScleroTrainer can build a practitioner's confidence, in addition to strengthening his or her technique.
Dr. Nelson used a prototype of the model to train her own Physician Assistant. The PA became proficient and "it was a breeze" when she sat down with her first real patient. The final product was shipped in October 2012, and a patent is currently pending. According to Dr. Nelson, one of the drawbacks of the ScleroTrainer may also be one of its benefits. Although the model feels like real skin, it's more difficult to pierce than real skin. Plus, the ScleroTrainer has straight veins, whereas real veins are "twisty and tortuous." When performing sclerotherapy, the clinician should look for the straight part of that vein that's going to incorporate the entire bevel of the needle; the ScleroTrainer teaches you what to look for.
"That's what you want with any training device," explained Dr. Nelson. "You want the person being trained to sit down to a regular person and say, 'this is much easier.'" Perhaps the greatest benefit that the ScleroTrainer offers is to get those performing sclerotherapy to trust their hands and not their eyes. When the needle goes into a tiny vein, people think that they're in the vein because it appears so, when in fact, they might be underneath the vein. Practicing on the model trains them to know what the proper resistance would feel like.
Early this year Dr. Nelson was recognized by Smart Business Magazine with a 2013 Innovation Award, but perhaps her biggest coup was at the recent World Meeting of the International Union of Phlebology. For years doctors have been teaching others the nuances of sclerotherapy using a cabbage leaf. This year, however, the training vegetable was supplanted by the ScleroTrainer at all of the sclerotherapy training courses. "I have ousted the cabbage leaf," said Dr. Nelson proudly. The ScleroTrainer currently retails for about $800 and is available at www.sclerotrainer.com or 440-616-6061. (A model that includes a magnifier with three lenses will be available in early 2014.)
Concerned about your vein health?
Contact the Vein Healthcare Center for an evaluation.
Contact Us