Cover Story
Women & Veins: Why Gender is a Risk Factor for Venous Disease
By Jennifer Boggs | Feature
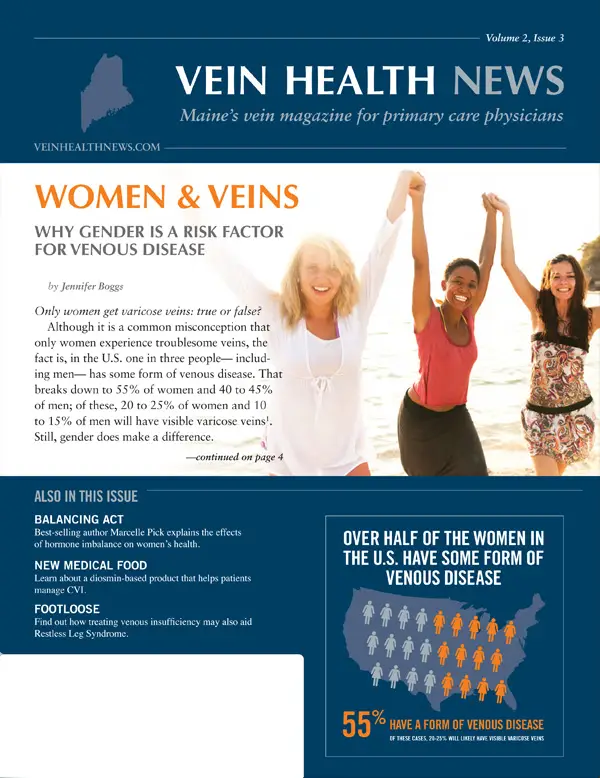
Only women get varicose veins: true or false? Although it is a common misconception that only women experience troublesome veins, the fact is, in the U.S. one in three people—including men—has some form of venous disease. That breaks down to 55% of women and 40 to 45% of men; of these, 20 to 25% of women and 10 to 15% of men will have visible varicose veins. Still, gender does make a difference.
Venous disease is defined as the impairment of blood flow back towards the heart. This occurs when healthy vein valves become damaged and the backward flow of blood "pools" in the legs or feet. Symptoms may present as discomfort, fatigue, or heaviness in the leg, causing varicose veins and other skin changes. Over time, the increased pressure can cause additional valves to fail. If left untreated, it can lead to extreme leg pain, swelling, ulcers, and other health problems.
Risk factors for developing venous disease, regardless of gender, include family history, age and inactivity. Another significant risk factor—fluctuations in hormones—is related to gender. According to Dr. Suzanne Jones, a board certified phlebologist and founder of Michigan Vein Care Specialists in Ann Arbor, a woman has three potential "high risk" times in her life that men do not. Significant hormonal fluctuations typically happen during menarche, pregnancy, and menopause. "At these times, hormone surges are very common for women," said Dr. Jones. "Progesterone can act as a vasodilator and cause the veins to stretch, sometimes enough for the valves to tear and subsequently fail." Women who have venous insufficiency will often notice that their symptoms worsen during menstruation, for example.
What to expect
About forty percent of pregnant women are likely to develop varicose veins. During pregnancy, a combination of hormonal changes—specifically, greater amounts of estrogen and progesterone—and increased pressure on the abdomen can cause varicose veins to manifest. Interestingly, the most damage seems to happen in the first trimester, so those with known risk factors for venous disease should be instructed to wear graduated compression stockings throughout the first three months of pregnancy and possibly longer. (See "Preventing varicose veins during pregnancy" sidebar.)
The volume of blood in a healthy woman increases by about 50% more than before the pregnancy, with the largest increase in the second trimester. With more volume to move, all of the blood vessels are under increased stress and veins can become very swollen. In the final trimester, the expanding uterus can put pressure on the inferior vena cava, and further restrict proper venous return to the heart. Pregnancy is also a time when women are more prone to blood clots, so phlebitis (inflammation of the walls of a vein that can cause a clot to form) can also be a concern.
It is not considered safe to treat varicose veins with aggressive treatments during pregnancy, advised Dr. Jones, but wearing good compression stockings can prevent them from getting worse and can go a long way toward relieving the symptoms. "During pregnancy, the two most important preventative things to consider are periodically elevating the legs and compression," she said.
After labor, most women who had significant venous disease during pregnancy notice a big improvement after the baby is born, but it doesn't always resolve completely. Dr. Jones suggested that if patients have symptoms that are persisting several months later, they should be evaluated and treated. "If a patient was uncomfortable because of her veins during the first pregnancy, then she should seriously consider seeking treatment between pregnancies—the next one could be pretty miserable if veins go untreated."
According to Dr. Jones, patients can be safely treated for varicose veins 6-8 weeks after delivery. Hormonal levels are back to normal within that time (if the patient is not breastfeeding), and water retention and any clotting risks have usually returned to baseline. Depending on the type of treatment, breastfeeding may be an issue for some patients. Treatments that require a local anesthetic, such as endovenous laser ablation (ELVA) or microphlebectomy, have been proven safe. Sclerotherapy is not recommended if the patient is breastfeeding, as certain medications used during this procedure have not been proven safe and may be excreted in breast milk. However, if the patient is willing to forgo breastfeeding for 24 hours, sclerotherapy is possible. Some vein specialists may recommend that women seek treatment for problematic veins before their first pregnancy, especially if there is a strong family history of vein issues.
The effects of aging
Even after menopause when most hormone fluctuations have stopped, a woman's risk of venous disease continues to increase with age. As the body gets older, a decrease in the production of collagen causes the veins to become weaker and the valves more likely to fail, especially in the superficial veins. For this reason, there is a higher incidence of varicose veins in the elderly population.
Older women may think varicose veins, or even leg ulcers, are a normal part of aging, but what many don't realize is that they don't have to live with symptoms. Even those who experience an aching or heaviness in their legs can receive treatment and relief. Treating the symptoms also arrests the progression of the disease. Treating the aching legs of a 60 year-old patient will improve her quality of life, and may also prevent an ulcer.
Post-menopausal patients who are taking hormone supplements should be aware of the increased risk of blood clots, which can damage veins or worse. Additionally, the incidence of deep vein thrombosis (DVT) is higher in older people because of the conditions described as Virchow's triad (endothelium damage, stasis, and hypercoaguability). DVT occurs when a blood clot forms in one of the large veins—usually one of the lower limbs, such as the thigh or calf—leading to either partially or completely blocked venous return. Physicians should consider recommending that their senior patients visit a phlebologist for a superficial venous evaluation prior to elective surgeries, especially hip or knee replacement. This step will help the patient learn her risks and decrease the chances of getting DVT.
Being proactive
Spider veins and varicose veins are health issues, but due to misinformation or dated attitudes, many women do not treat them as such. Dr. Jones believes that it's important for women to be aware of venous disease and its symptoms and, as with any illness, to know the family history. (Someone with first-degree family members with vein issues, for example, will find her risk is significantly increased.) Primary care physicians can be a great help to their female patients by: 1) listening to their concerns about their legs and veins, and 2) being knowledgeable about measures to treat and prevent venous disease.
With the right information, women have the ability to reduce their risk of developing venous disease and/or decreasing its severity. Preventative measures include: elevating the affected leg above heart level; wearing graduated compression stockings; living an active lifestyle, maintaining a healthy weight; and avoiding tight-fitting clothing and high-heeled shoes. "Treatment of venous disease has progressed drastically in the last several years," added Dr. Jones. "Countless women have watched their mothers' and grandmothers' legs become terribly painful and unsightly, but that doesn't have to be their destiny."
SOURCES
- Varicose veins and venous insufficiency. Society of Interventional Radiology web site. http://www.sirweb.org/patients/varicose-veins/. Accessed June 12, 2013.
Pregnancy
Preventing Varicose Veins During Pregnancy
By Vein Health News Staff
A woman's body goes through many changes during pregnancy, including an increase in blood volume and fluid. Fluid retention often causes swelling in the legs, ankles and feet. Graduated compression stockings promote circulation and venous efficiency, which helps to reduce swelling and pain—and, in many cases, can prevent or minimize varicose veins.
Ideally, any woman with a positive family history should wear full-length stockings (or at least knee-high stockings) throughout her entire first trimester. Stockings come in a variety of styles and strengths, from knee-highs and thigh-highs, to full-length stockings. For pregnant women, there are even panty hose styles with more room in the belly, specially designed to expand during pregnancy without restricting the abdomen. They are graded on the basis of the strength of the compression at the ankle. Commonly prescribed strengths include: 15-20 mmHg for spider veins or patients with varicose veins but only mild symptoms or swelling; 20-30 mmHg for mild to moderate varicose veins; and 30-40 mmHg for patients with varicose veins associated with symptoms such as pain and swelling.
Maternity graduated compression stockings are specially designed to fit more snugly at the ankles and calves and less so toward the top. The gradual change in compression helps the weak valves in the veins to circulate the blood more effectively. Though pregnancy compression stockings (and body garments) are available with a doctor's prescription, many maternity stores also offer them. Accurate sizing is critical, so it is best to check with a doctor prior to purchasing any type of compression while pregnant. "If a patient tries one and doesn't like it, she shouldn't give up," said Dr. Suzanne Jones of Michigan Vein Care Specialists. "These days there are so many styles and strengths to choose from."
Health
Finding Balance: A Holistic Approach to Women's Health
By Jennifer Boggs
Marcelle Pick knows a thing or two about hormones and women's health. Pick, an OB/GYN Nurse Practitioner, is the author of the book Is It Me or My Hormones? and cofounder of the Women to Women Clinic in Yarmouth, Maine. In her practice, she undertakes an integrative approach, which treats illness and helps women make choices in their lives to prevent disease.
Some of the most difficult health challenges in a woman's life occur during intense hormonal shifts, such as pre-menstruation, menstruation, pregnancy, perimenopause and menopause. "Hormonal imbalance is a real phenomenon with very real symptoms, but there are also practical actions that women can take to feel better and be well," said Pick.
The number one action on Pick's list is eating the right kind of food. According to Pick, people's diets have changed radically in the last twenty years—and not for the better. She named processed foods and increased intake of sugar and carbohydrates as the biggest culprits of systemic inflammation. "If we have a set of genes and feed them the wrong nutrients, a.k.a. 'information,' it can turn the gene on or off and cause an inflammatory cascade, which is at the root of many diseases and immune disorders," added Pick.
Stoking inflammation
Acute inflammation is the short-term immune response that the body needs to fend off physical threats, such as trauma, infection, or allergy; pro-inflammatory compounds are released, followed by anti-inflammatory compounds once the threat has been resolved. If this response is not completely "turned off" and continues to stimulate pro-inflammatory immune cells that circulate throughout the system, then the result is chronic inflammation.
Pick explained that inflammation is especially significant for women in perimenopause and menopause, because these major hormonal disruptions seem to make inflammation worse. Reducing inflammation, then, can help stabilize a patient's hormones and make these transitions easier.
To counter inflammation Pick suggested revising one's diet by limiting or eliminating certain foods and additives—trans fats, sugars, and refined carbohydrates especially—and replacing these with antioxidant-rich fruits and vegetables, wild seafood, and food containing healthy fats, such as omega-3's and olive oil. A high-quality multivitamin-mineral complex, as well as probiotics (in supplement form or found naturally in certain foods), help rebalance the immune system.
As a practitioner of functional medicine, Pick understands deeply the role of lifestyle choices in restoring and maintaining good health, through regular exercise, adequate sleep, and reduced stress.
Natural approach to veins
Veins are just one part of the body's complex system, but as with the body as a whole, Pick looks for natural ways to help symptoms of venous disease. In addition to overall dietary changes, she will recommend that patients with vein issues increase their intake of foods with rutin (also known as rutosides), a citrus flavonoid glycoside found in buckwheat, asparagus, cherries, berries, and the rinds of some citrus fruits. Rutins have been found to improve circulation, strengthen capillaries, reduce inflammation, and improve venous edema.
Horse chestnut (the common name for aesculus hippocastanum) is an anti-inflammatory herb that has been found to promote normal tone of the vein wall, thereby improving circulation through the veins. Butcher's broom (or ruscus aculeatus) is another effective herb with positive effects on blood flow.
Although Pick has found these supplements to be effective for many patients, she emphasized: "it's not one size fits all." As for lifestyle modifications, Pick mentioned exercise and maintaining a healthy weight as keys to good vein health. She also encouraged women with vein problems to avoid high heels and tight, restrictive clothing—which can impede proper circulation. "Each one of us has a weakened part of our body, but if you start to pay attention and take responsibility for your body and your lifestyle, you'll start to see miracles," said Pick. "That goes for varicose veins, that goes for your overall health."
FAVQ
Is Restless Leg Syndrome Vein-Related?
By Dr. Cindy Asbjornsen
The short answer is that we're not exactly sure. In fact, a single unifying cause of Restless Leg Syndrome (RLS) has yet to be established. We do know is that there are many potential causes for RLS, including pregnancy, diabetes, and rheumatoid arthritis, not to mention medications such as antihistamines, anti-depressants, and a certain class of high blood pressure medicine.
RLS is considered a disruptive neurologic disorder, affecting approximately 10 percent of the U.S. population. It occurs in men and women, though the incidence is twice as high in women. RLS is not diagnosed through laboratory testing, but rather through evaluation of symptoms. According to the International Restless Legs Syndrome Study Group, the four primary features of RLS are: An urge to move, usually due to uncomfortable sensations that occur primarily in the legs; Motor restlessness (expressed as activity) that relieves the urge to move; Worsening of symptoms by relaxation; Variability over the course of the day-night cycle, with symptoms worse in the evening and early in the night.
About 40 percent of people with RLS have problems with their veins, but we don't fully understand the relationship between RLS and venous disease. Research shows that there is high correlation of patients who see their RLS resolve when they receive venous treatment. One study showed that treatment of venous reflux eliminated or significantly reduced 98 percent of a person's RLS symptoms. (Ninety-two percent of symptoms did not return after one year.) Despite this study and others, there are currently no prospective random clinical trials that show that RLS is directly related to veins.
It is worth adding that many phlebologists have found that when patients wear graduated compression stockings, their RLS symptoms improve. There is no cure for RLS, but many treatment options are available to help manage symptoms, including long-term use of prescription medication. In my own experience, I've had patients tell me that treatment for venous insufficiency has completely relieved their RLS and others who saw no difference at all. But research findings and anecdotal evidence suggest that the patients who are evaluated for restless legs syndrome would benefit from an evaluation for possible vein disease as well. An article in the journal Phlebology (2008;23:112-117), for example, concludes that all RLS patients should be properly evaluated for venous reflux before initiation or continuation of drug therapy.
Patient Perspective
One Patient's Perspective: All in the Family
By Benjamin Lee
In the 1950s, most women wore dresses and skirts, but Priscilla's mother always wore pants to cover up her bulging, unattractive veins. Her mother's legs were so swollen that her knees disappeared, her legs as wide at the bottom as at the top—what people used to refer to as "stump leg." "The worst thing was that when my mom got into her 70s and 80s, her varicose veins were so painful she could barely move," said Priscilla. "She was a very active woman who became so limited because of her legs."
Priscilla, who lives in New Hampshire, has had her own venous challenges. Shortly after her daughter Stacie was born, she sought treatment for her increasingly painful varicose veins. The only option available at the time was vein stripping, which she described as "quite a process." The treatment proved effective for about 18 years, but then Priscilla's legs and ankles began to swell again, and the heaviness and discomfort returned. Sometimes the pain was so bad that she couldn't walk or stand for very long: "Every time I sat down I would have my legs raised. I'd get tired of telling people, 'my legs bother me today.'"
Priscilla knew she had to do something or risk ending up like her mother. After researching vein treatment online, she found a board certified phlebologist and made an appointment to be evaluated. She was fascinated to learn about the new technologies that were available. "I was under the assumption that once veins are stripped you can't do anything else, she said. "I was elated to find out that I had other options and something more could be done!"
Priscilla determined that her main goal was relief from the pain and swelling. Together with the vein specialist, she decided to have endovenous laser ablation (EVLA) for both legs, followed by sclerotherapy. Since then she goes to the local Y to exercise "every single day," something she would never have dreamed of just a few years ago. One small drawback, according to Priscilla, is bruising. She said her skin is very fair and sensitive, so after treatment, including sclerotherapy, she would get some bruising. Other than that, Priscilla has been thrilled with the outcome.
Like mother, like daughter
Since vein disease tends to run in families, "bad veins" didn't end with Priscilla. Her 42 year-old daughter Stacie also has chronic venous reflux. Stacie began to see symptoms in her mid-twenties, but because of her mother's (and grandmother's) family history, she was aware of the problem and did her best to take care of it. She started doing sclerotherapy, but when she got pregnant in her 30s, her veins got worse.
"The sclero would work for awhile, then the veins would come back," said Stacie. She then underwent radiofrequency (RF) ablation, but that didn't work either, so she switched doctors. Her new doctor performed ligation for the purpose of shutting down both her saphenous veins. Post-surgery she felt instant relief, but almost six months later she experienced full reflux: "It felt like I'd had no treatment at all, and none of the valves in my veins seemed to work." A second round of RF also yielded results, but six months later "everything re-opened again." After her doctor retired, Stacie visited a third doctor who removed both of her saphenous veins from ankle to groin. Yet, she still felt no relief.
"It's disheartening when you're veins are stripped and it's still not taken care of," shared Stacie. "There were nights I couldn't sleep, it was so painful." Fortunately, Stacie's mom had already started treatment with her phlebologist and recommended that Stacie pay her a visit. After an ultrasound evaluation, they found the root of the problem. Since then she's had EVLA on her left leg, along with a significant amount of sclerotherapy. The follow up and possible treatment will be ongoing because the past difficulties she's had with her veins. Stacie feels much better than prior to her last treatment, though she still gets an achy feeling on occasion. And compared to what her legs looked like before, they also look better.
Speaking from experience
Both Priscilla and Stacie agree that anyone seeking treatment for their veins should look for someone who is trained in vein care specifically. Priscilla added that it helps to find a vein specialist who is passionate about what he or she does and "really understands how debilitating it can be." Stacie's has some advice for younger women with vein problems: "I was in my mid-20s when I was first affected, so don't think it's just an 'old lady' kind of thing." She also suggests that those who have relatives with vein disease take special care. "Don't wait. It's not something to put off, because it does get progressively worse and it won't go away on its own," she said. "If you have a family history, you need to stay on top of it."
Vein Tech
Vasculera
By Benjamin Lee
Interest in alternative options for preventing and treating chronic venous insufficiency continues to grow. One such option is diosmin, a naturally occurring flavonoid that can be isolated from plant sources such as citrus, or derived from a related flavonoid called hesperidin, which is found primarily in certain types of oranges and grapefruit. (Flavonoids are a large class of plant-based molecules that act as antioxidants and anti-inflammatory agents.)
Vasculera™ is a once-a-day tablet that contains diosmin and is indicated for the clinical dietary management of chronic venous insufficiency (CVI) and its complications. Primus Pharmaceuticals, Inc. made the prescription medical food product available in the United States about a year ago. According to Robert Levy, M.D. and Director of Clinical Development at Primus, diosmin has been marketed in Europe for almost 30 years, under the brand name Daflon, among others.
Dr. Levy said that diosmin is an "extraordinarily well-studied molecule" with hundreds of published papers and dozens of clinical trials with more than twenty thousand subjects participating over the years. "The literature shows that response for all components of CVI is in the range of 85-90%, and improvements have been seen in venous tone, capacity and flow, lymphatic flow and CEAP classification, as well as symptoms," he said.
The diosmin in Vasculera (diosmiplex) helps manage several forms of CVI, including varicose veins, spider veins, edema, lymphedema, stasis dermatitis, and even venous ulcers. It does this by increasing venous tone and lymphatic drainage, while decreasing the production of adhesion and inflammatory molecules that are created due to elevated venous pressure and venous acidosis. Dr. Levy described it as a vicious cycle: "CVI causes vein pressure to increase, which activates the endothelial cells in the veins (creating adhesion molecules) and localization of white cells in tissues. The resulting inflammation further damages the vein wall and, eventually, the vein valve, causing venous pressure to rise and activate more adhesion molecules."
The product also acts to decrease the acidic environment that develops in veins when blood flow is slowed due to venous hypertension. In addition to diosmin, Vasculera contains a proprietary alkalinizer called Alkaplex, which has been shown to resist neutralization by acid solutions in the stomach. According to Dr. Levy, because only a small portion of the alkaline salts are neutralized in the stomach, the rest is transferred to the small bowel and are absorbed into the blood, rendering the product more effective. "The combination of these two components reduces the cycle that perpetuates CVI symptoms and promotes healthy venous tone and blood flow," said Dr. Levy.
Company data states that results may appear in as little as one week but may not be seen for 4 to 8 weeks; for venous ulcers, results may not be seen for several months. Side effects are relatively minor, the most common being mild upper gastrointestinal discomfort which occurs in about 5% of users but tends to clear after a short period of use. According to the company, the product is applicable in a variety of clinical settings. For example, hemorrhoids—basically, varicose veins in the ano-rectal area—are another manifestation of CVI. Vasculera has been prescribed for the treatment of acute and chronic hemorrhoids.
Dr. Levy reported that there have been unexpected potential indications that the company is beginning to study, including pelvic congestion syndrome in women. Anecdotal accounts—including one from a gastroenterological nurse—have suggested that Vasculera can help diminish the uncomfortable symptoms that occur when pelvic veins (such as in the ovary or uterus) become inordinately dilated. Dr. Levy is now conducting clinical trials in this area.
Vasculera is contraindicated for anyone having a hypersensitivity to any of its ingredients, especially those allergic to citrus. It is not recommended for pregnant or lactating women or patients with a history of cancer, since there has not been appropriate research conducted in these patient populations. Though a medical food, Vasculera must be prescribed a physician. Most pharmacies have access to Vasculera through their individual distributors.
Concerned about your vein health?
Contact the Vein Healthcare Center for an evaluation.
Contact Us